By Pat Anson, PNN Editor
One of the pioneers of pain management in the United States is hoping to draw more attention to intractable pain and how it differs from chronic pain. While chronic pain lasts for 90 days or more, intractable pain can persist for years, decades or even a lifetime. Many doctors fail to distinguish between the two, which leads to gaps in diagnosis and treatment.
“The pain field has been woefully negligent about this. They talk about symptomatic treatment of what to do to relieve chronic pain, but in order to deal with intractable pain syndrome you’ve got to treat the underlying cause,” says Dr. Forest Tennant, whose foundation has just released a new report called “The Intractable Pain Syndrome: A Call for Recognition and Prevention.”
“We’ve worked on it for quite some time with the goal of having every patient, doctor, nurse and family understand it. And to try and bring things out in language that is understandable by everybody.”
“This was a labor of love for all of us, born from a sincere desire to bring recognition, treatment and prevention to this devastating syndrome,” says co-author Ingrid Hollis, whose son was treated by Tennant for Arachnoiditis and Ehlers-Danlos Syndrome. “We have learned so much through the years, and I believe there is much that can be done to prevent intractable pain syndrome from developing and progressing when it occurs.”
“One of the reasons we’re doing this is to call for early recognition and vigorous treatment,” Tennant told PNN. “Someone who has this for two, five or twenty years, you can’t expect much reversal. But those people who have these conditions for six months or a year, they have a great ability to reverse a great deal of this. The earlier the treatment, the better the outcome.”
Left untreated, Tennant says intractable pain syndrome (IPS) can lead to chronic inflammation in the central nervous system that is difficult to reverse. The inflammation not only causes constant pain, it leads to loss of brain tissue and creates dysfunction in the neurologic, cardiovascular, hormone and immune systems.
“We’ve known for centuries that a painful injury will create what amounts to electricity. And too much electricity causes inflammation and inflammation causes tissue destruction,” says Tennant. “Intractable pain syndrome does change their basic physiology by virtue of altering physically the neurotransmitter systems that are in the brain and spinal cord. That is really the difference. And this is very objective. It’s measurable. It’s visible. It’s clear when its present.”
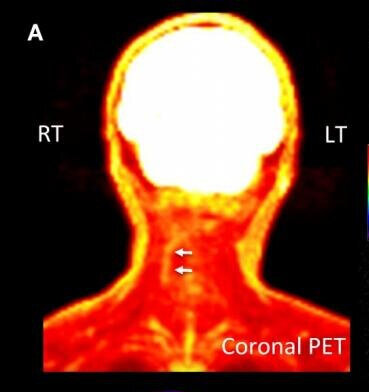
Tennant says these “pockets” of inflammation can be seen on MRI’s and brain scans. Someone suffering from simple chronic pain won’t have them, but people with intractable pain will.
There are five basic conditions that can cause IPS:
Arachnoiditis, a chronic inflammation of spinal nerves
Genetic connective tissue/collagen disorders such as Ehlers-Danlos Syndrome (EDS)
Reflex Sympathetic Dystrophy (RSD), also known as Complex Regional Pain Syndrome (CRPS)
Brain injuries caused by strokes or head trauma
Serious end-stage osteoarthritis of the spine, hips, knees or feet.
Other possible causes of IPS are porphyria, sickle cell disease, Lyme disease, interstitial cystitis, and some rare genetic disorders.
IPS Can Be Reversed
Long recognized as incurable, Tennant says intractable pain can be reversed if diagnosed and treated early. He has pioneered some new treatments for IPS, including hormone supplements, physical therapy and better nutrition.
“Our project hopes to educate people about what they can do to reverse a lot of this,” Tennant told PNN. “Step number one is you’ve got to have vigorous treatment of the underlying cause of pain. The arachnoiditis has to be treated. The arthritis has to be treated. The RSD has to be treated. In other words, vigorous treatment of the underlying condition.
“Step number two, there are specific things they can do to slow down the inflammation inside the central nervous system. We know the body makes hormones inside the brain and spinal cord that can reduce the inflammation inside the central nervous system and regrow some of the tissue that’s been lost. People say you can’t do that, but oh yes, you can. There are studies that show this and we see this clinically.”
“I strongly believe that Dr. Tennant's concept of how intractable pain develops and progresses is absolutely correct. His work in identifying the causes, developing diagnostic criteria, and figuring out a treatment protocol provides what doctors need to know to help people with intractable pain,” says co-author Kristen Ogden, whose husband Louis was treated by Tennant for a complex autoimmune condition.
“Louis' treatment with Dr. Tennant allowed him to improve so much in so many ways. Very effective pain control, greatly improved function and the best quality of life he ever had as an adult. I am sure that very few people have any idea at all how much a seriously ill pain patient can improve and even regain lost function and capabilities if they have the right medical regimen that meets their needs.”
Tennant retired from clinical practice in 2018, the year after his home and office were raided by the DEA as part of an investigation into his opioid prescribing. No charges were ever filed against him. While Tennant no longer sees patients, he is continuing his research into the treatment of IPS – which notably downplays the use of opioids.
“The answer to opioid use is treating the syndrome rather than just giving symptomatic relief. Opioids are symptomatic drugs,” explains Tennant. “What we’re saying is, identify this and try to treat the condition. Don’t just throw a bunch of symptomatic antidepressants, opioids and other interventions at it. Start trying to look at it physiologically and pathologically, and treat it like we do other syndromes.”
To learn more about the Tennant Foundation’s Intractable Pain Syndrome Research and Education Project, click here.
Dr. Tennant and the Tennant Foundation have given financial support to Pain News Network and are currently sponsoring PNN’s Patient Resources section.