Most Treatments for Low Back Pain Don’t Work
/By Crystal Lindell
While I’ve struggled with relatively mild lower back pain for years now, a few months ago I threw my back out for the first time. I literally could not get out of bed on my own, and I spent almost a week on the couch recovering while my lower back spasmed.
It was horrible, and even my usual pain relief methods and doses of pain meds did not help much. In the end, for me, it was mostly just time and rest that seemed to help the most.
Now a new study confirms just how difficult it is to treat low back pain.
In fact, only about 10 percent of treatments for low back pain actually work, according to new research published this week in the journal BMJ Evidence-Based Medicine.
The study by an international team of researchers looked at 301 placebo-controlled clinical trials for 56 different treatments for low back pain. The team found that most non-surgical and non-interventional treatments did not work. Those that did work provided only small analgesic effects better than a placebo.
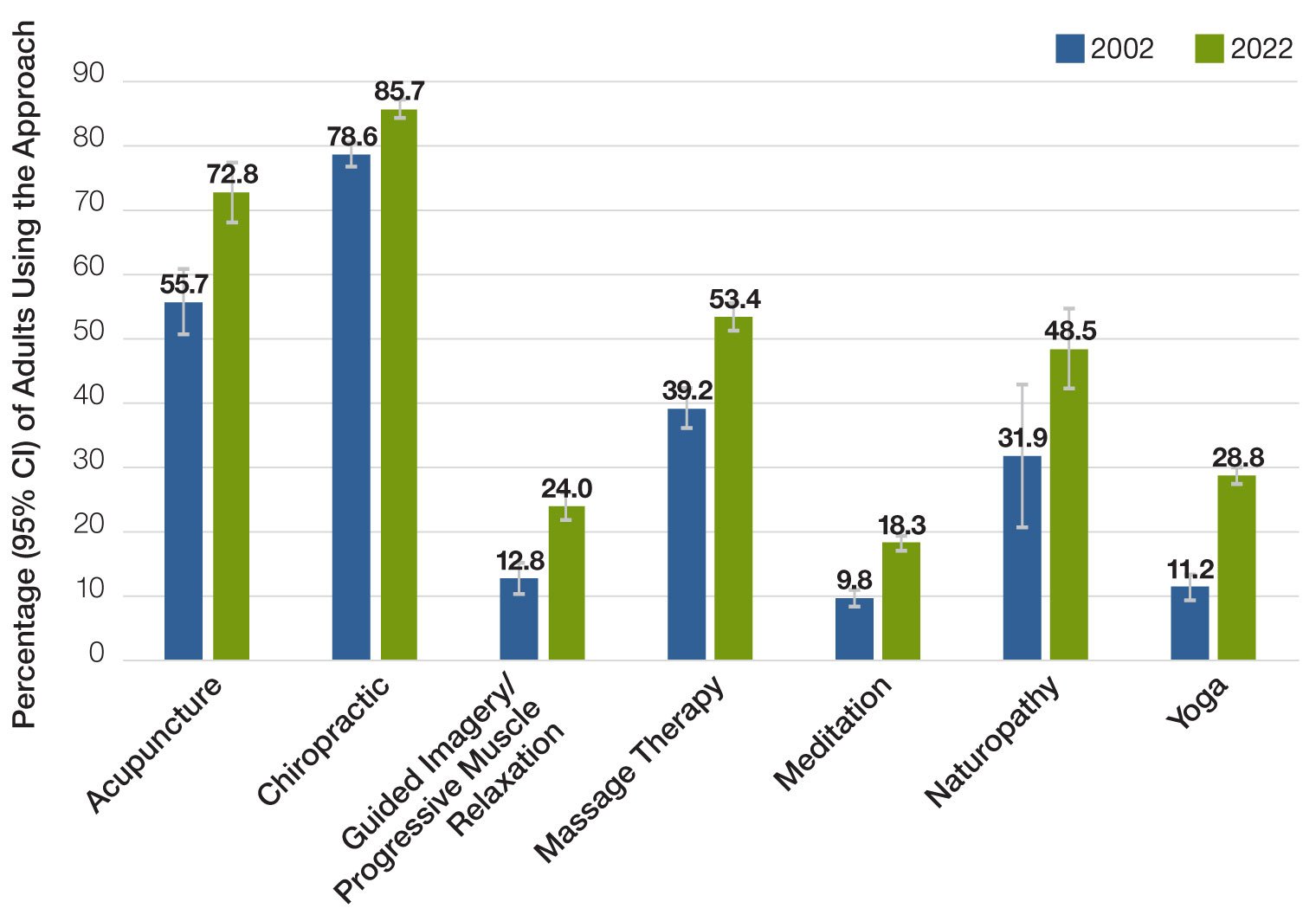
Specifically, they found that NSAIDs were the only treatment that worked for acute low back pain, while five treatments for chronic low back pain provided relief: exercise, spinal manipulative therapy (chiropractic), taping, antidepressants, and transient receptor potential vanilloid 1 agonists, which are topical patches like Qutenza (capsaicin).
As for the treatments that did not work, the researchers found that three treatments for acute low back pain – exercise, glucocorticoid injections, and paracetamol (acetaminophen) – and two treatments for chronic low back pain (antibiotics and anaesthetic drugs) were ineffective.
They didn’t have enough good quality evidence for the remaining treatments to determine if they worked or not.
For acute low back pain, 10 non-pharmacological treatments had “low to very low certainty evidence” that they actually worked, including: acupuncture, behavioral health education, extracorporeal shockwave, heat, laser and light therapy, massage, mobilization, osteopathic, spinal manipulative therapy, and transcutaneous electrical nerve stimulation (TENS).
They also found that 10 pharmacological treatments had inconclusive evidence about their effectiveness for acute low back pain, including: cannabinoids, colchicine, immunoglobulin, muscle relaxants, muscle relaxants + NSAIDs, nucleoside, opioids, ozone injections, pyrazolone derivatives, and topical rubefacients.
For chronic low back pain, over three dozen treatments had inconclusive evidence to support their efficacy, which included everything from bee venom and TENS to dry cupping and muscle relaxants.
The bottom line is that there’s not much evidence to support the use of many treatments that are commonly prescribed and promoted for lower back pain — even the ones recommended in medical guidelines.
“Our review did not find reliable evidence of large effects for any of the included treatments,” researchers concluded. “There are also common treatments for which no placebo-controlled trials have been conducted despite being commonly recommended in clinical practice guidelines.”
The study ends as many often do, with a plea for more high-quality evidence to give patients and doctors real choices and effective options for treating back pain.
“While we would like to provide more certain recommendations for where to invest and disinvest in treatments, it is not possible at this time,” researchers said.