Americans Are Using More Alternative Pain Therapies
/By Pat Anson, PNN Editor
It’s fair to say that almost every person living with chronic pain has been told by a doctor, loved one, friend or even strangers that they should try a “complimentary health approach” to pain management. Also known as a “multimodal” or “comprehensive” care, the idea is to get pain patients to reduce or stop using opioids and other medications by utilizing alternative health therapies such as massage, meditation and acupuncture.
A new study shows that there has been surge in the use of those therapies by Americans over the last two decades, with chronic pain sufferers leading the way.
Researchers at the National Institutes of Health looked at data from the 2002, 2012, and 2022 National Health Interview Survey (NHIS) to evaluate the use of seven alternative therapies: yoga, meditation, massage, chiropractic care, acupuncture, naturopathy, and guided imagery/progressive muscle relaxation.
Their findings, published in JAMA Network Open, show significant increases in the use of all seven therapies. The most widely used alternative therapy was meditation, which rose from 7.5% of respondents in 2002 to 17.3% in 2022.The largest increase in utilization was for yoga, which rose from 5% of respondents in 2002 to 15.8% in 2022.
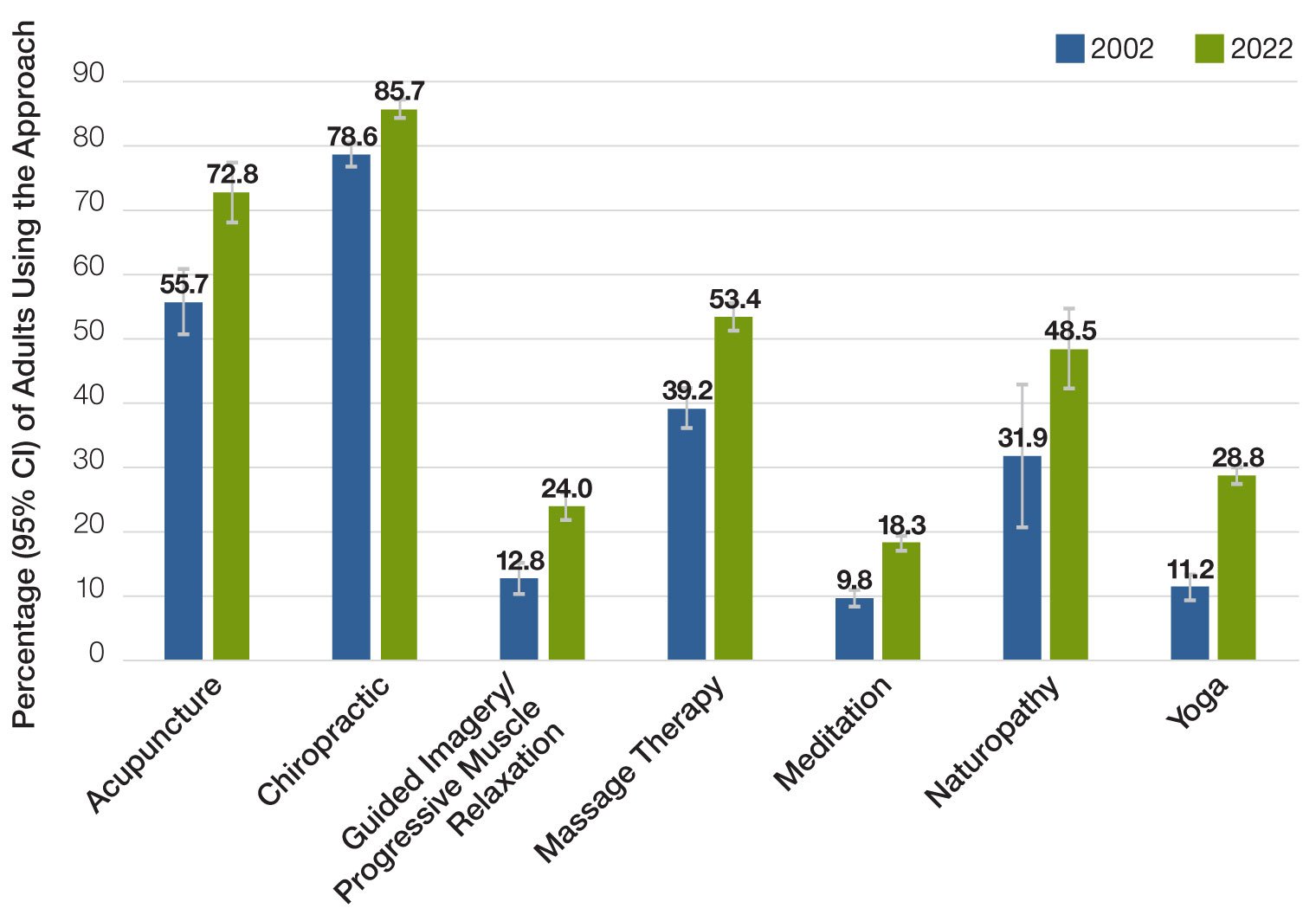
Complimentary Health Approaches Used by U.S. Adults
NATIONAL INSTITUTES OF HEALTH
By 2022, over a third of respondents (36.7%) reported using at least one complimentary health approach (CHA), up from 19.2% in 2002. Nearly half said they used a CHA for pain management.
The CHAs most widely used for pain in 2022 were chiropractic care (85.7%) and acupuncture (72.8%). Researchers think that expanded insurance coverage for those treatments may have contributed to their growing use. Significant reductions in opioid prescribing over the last decade may have also driven people to try other treatments.
Complimentary Health Approaches Used for Pain
NATIONAL INSTITUTES OF HEALTH
“Between 2002 and 2022, US adults increasingly used CHAs, including for pain management. This shift in utilization coincides with increased pain prevalence nationally and may be attributable to several factors, including randomized clinical trials suggesting that some CHAs provide low to moderate levels of pain management, incorporation of CHAs into best practice pain management guidelines, and the need to mitigate unnecessary use of potentially harmful opioids through use of nonopioid interventions,” wrote lead author Richard Nahin, PhD, lead epidemiologist at the National Center for Complementary and Integrative Health.
As with many of these data mining studies, the NIH researchers did not document what kind of pain conditions the respondents had, how often they used an alternative therapy, or even whether the treatment worked.
According to one estimate, 55 million U.S. adults spent $28.3 billion on CHAs in 2012, about 9% of total out-of-pocket health care expenses that year.