An Open Letter to President-Elect Trump
/By Percy Menzies, Guest Columnist
Dear President-Elect Trump,
You will soon have an extraordinary opportunity to save thousands of lives with one stroke of the pen! I am talking about reducing overdose deaths from opioid overdoses. How is this possible?
We have three highly effective medications for the treatment of opioid addiction, but they are grossly under-utilized, largely due to accessibility. Two of the three drugs used to treat opioid use disorder have restrictions that have no place when overdose deaths exceed 30,000 per year. These restrictions made sense at a different time, but these barriers are now inadvertently contributing to overdose deaths.
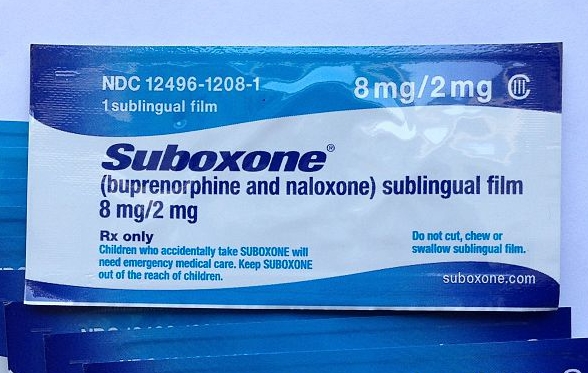
I am specifically talking about buprenorphine, the most widely used medication in the battle against the opioid epidemic. This medication, better known by its brand name Suboxone, is an opioid with a very safe profile. Its unique pharmacology makes it almost impossible to overdose.
There are barriers to the use of this medication which made sense 14 years ago, when heroin was not a public health issue, but today they are a hindrance to saving lives.
Buprenorphine is the only drug that requires physicians to complete eight hours of training and then apply to the Drug Enforcement Administration to obtain a special exemption to prescribe it. It gets worse. Physicians can only treat 30 patients with this medication in the first year, and then they must obtain permission from the DEA to increase the limit to 100 patients. The physician also has to keep clear records and can expect a visit from a DEA agent to look at the records.
This is a major deterrent and way too few physicians have bothered to obtain the required exemption. Any physician who has a DEA license can prescribe an FDA-approved controlled substance without restriction, but they have to deal with this barrier to prescribe buprenorphine.
These restrictions were put in place to prevent buprenorphine from joining the opioid “pill mills” when few anticipated heroin sweeping our cities and towns. At the present time, there is no strategy in place to cut off or curtail the supply of heroin, or heroin that is laced with super potent opioids like fentanyl. Deaths from prescription opioids are declining, while deaths from heroin and fentanyl are climbing. Indeed, prescriptions for opioids drugs have fallen between 12 -25%, but the overdoses deaths have not declined.
Yes, buprenorphine is being diverted, but most experts believe that is due to the lack of treatment. Patients desperately seeking treatment are purchasing the drug on the streets. Many experts believe that if patients have expanded and easier access to buprenorphine, the diversion will drastically reduce and more patients will be in treatment and get away from heroin.
Several steps have been taken to address this catastrophic problem, but these steps are woefully inadequate. Expansion of the needle-exchange programs and the widespread distribution of the opioid overdose drug naloxone (better known by the brand name Narcan) are welcome and should be expanded, but they are at best palliative in nature. These measures do little to address the underlying addiction.
The federal government is increasing the patient limits for buprenorphine for selected specialists from 100 to 275, and will also allow nurse practitioners and physician assistants to complete the required training and obtain the DEA exemption to prescribe buprenorphine. These are welcome steps, but fall far short of the response required to expand treatment and reduce deaths.
You got elected on a law-and-order platform and a promise to reduce the flow of heroin coming in from Mexico. Almost 50 years ago, Richard Nixon got elected on a similar platform. He too faced an unprecedented public health epidemic of heroin addiction – one that is nowhere close to what we are facing today.
President Nixon is remembered for taking a bold measure, which at that time was controversial. He initiated the opening of methadone clinics, which for the first time provided evidence-based treatment for heroin addicts. This measure reduced overdose deaths, protected society from criminal activity, and allowed these patients to become productive members of society. For the first time in the dark and checkered history of our nation, addiction was treated as a chronic healthcare issue and not a criminal activity.
Nixon went a step further to curb the supply of heroin coming into this country. He put political pressure on France to shut down the illegal labs processing Turkish-grown opium into heroin. Turkey also complied with the strong U.S. demand to curb the illegal cultivation of opium. Who can forget The French Connection, the thriller movie about this operation.
Mr. Trump, you have an extraordinary opportunity to lift the present restrictions on buprenorphine through executive order, to lure patients away from heroin and drastically reduce overdose deaths. Your action would provide increased treatment and not just palliative care.
Furthermore, you are in the best position to bring pressure on Mexico to eliminate the opium processing labs and drastically reduce heroin coming into this country. An epidemic is best treated when effective treatment is combined with eliminating factors contributing to the spread of the epidemic. In this case, it is the supply of heroin.
This one single action will earn you the gratitude of tens of thousands of families terrified at hearing a knock on the door informing them of the death of a loved one. You will also earn the gratitude of millions of patients suffering from chronic pain, who have been needlessly cut off from prescription opioids because of the overreaction of regulators and many physicians.
You will be remembered in history for a bold action that saved a generation from succumbing to a man-made epidemic.
Percy Menzies, M. Pharm, is the president of the Assisted Recovery Centers of America, a treatment center based in St Louis, Missouri.
He can be reached at: percymenzies@arcamidwest.com
The information in this column should not be considered as professional medical advice, diagnosis or treatment. It is for informational purposes only and represents the author’s opinions alone. It does not inherently express or reflect the views, opinions and/or positions of Pain News Network.