We Must Overcome Stigma Against Buprenorphine for Pain
/By Dr. Stefan Franzen
For years I had a negative impression of buprenorphine as a pain medication, both from personal descriptions I had heard by pain patients and from the scientific and medical literature.
I have since learned that buprenorphine can be effective pain reliever. At a high dose, the efficacy is similar to that of high-dose morphine or oxycodone, which were once commonly used to treat chronic or intractable pain.
Today, high doses of any opioid are shunned by most doctors because they are subject to increased scrutiny by state medical boards or even investigation by the Drug Enforcement Administration. The medical and moral justification of alleviating patient suffering appears to be irrelevant to public health authorities, even when they profess to favor a humane policy to treat pain.
We need a more rational discussion about opioids. Buprenorphine is an opioid that, when used alone, can play a role in pain treatment. Buprenorphine was developed in the United Kingdom in the 1960s and has been used in many countries to treat pain since the 1980s.
We must distinguish pure buprenorphine from Suboxone, which is a combination of buprenorphine and naloxone. Suboxone is given to people with opioid use disorder to help prevent abuse. If a tablet is crushed, extracted or injected by a drug abuser, the naloxone will block the effects of buprenorphine. However, if taken as directed under the tongue, the naloxone has much lower bioavailability.
A pain patient does not necessarily need naloxone and, depending on individual differences in body chemistry, the naloxone may even have negative effects. There is no reason to prescribe Suboxone for pain. It’s use as a pain medication is highly inappropriate, but may be the result of doctor’s fear of DEA action.
Pure buprenorphine is a different matter.
The CDC’s 2016 opioid guideline recommended that daily opioid doses not exceed 90 morphine milligram equivalents (MME). Although voluntary, the guideline was seized upon by other federal agencies and state legislatures to justify draconian new laws and regulations that limited opioid doses to 90 MME or less.
No such limits have been set for buprenorphine. However, few doctors in the U.S. prescribe buprenorphine for pain, despite recent studies demonstrating its efficacy and international recognition that it is an effective analgesic.
For historical reasons, American doctors do not know much about buprenorphine as a pain medication. Moreover, many fear prescribing any opioid in today’s regulatory climate. Patients know that buprenorphine has been used to treat addiction and therefore are suspicious of it as a pain treatment. They are also justifiably concerned about being stigmatized as a drug abuser if they are prescribed Suboxone.
U.S. Opioid Policy Lacks Common Sense
In short, the stigma surrounding buprenorphine is a significant factor preventing development of a rational opioid policy in the U.S.
Many patients with experience taking morphine, oxycodone, hydrocodone and other opioids say they are safe and non-addictive. Research shows that is true for a great many pain patients. However, a small fraction of the population is susceptible to opioid abuse and addiction. This is a classic ethics problem.
Should we let 99% of patients suffer because 1% might harm themselves? How do other societies manage this problem? We know what doesn’t work. The “War on Drugs” has been an unmitigated disaster for everyone: drug abusers, doctors, pain patients and their loved ones. Our drug overdose rate is 15 times higher than that the of European Union.
Worse still, our medical system and corporate regulation appear to lack common sense guardrails needed to prevent the diversion of prescription opioids -- even after massive publicity, sensational books, documentaries, and popular miniseries on the opioid crisis.
In case anyone had any doubt, the book “American Cartel” shows that diversion was mainly practiced by large opioid distributors and a few manufacturers, who flooded vulnerable communities with prescription opioids. Theft and deception of doctors by drug abusers also contributed to diversion. Each of these could be controlled in a sensible way, without forbidding people in pain from receiving medication. Yet, at present it appears there is no political will in the U.S. to even treat pain, regardless of the suffering of millions.
Instead, the politicians and media blame opioid prescribing, which implicitly blames doctors and patients. Perhaps as a response to this seemingly hopeless situation, a growing number of medical researchers have begun testing pure buprenorphine for the treatment of pain.
After seeing the effectiveness of buprenorphine, which I discuss in my new book, “Z’s Odyssey,” I became convinced that it is a viable treatment for even severe, intractable pain. This should be a choice, but the problem today is that many patients do not have a choice.
Pure buprenorphine for pain was not available in the United States until 2010, when the low-dose Butrans skin patch became available.
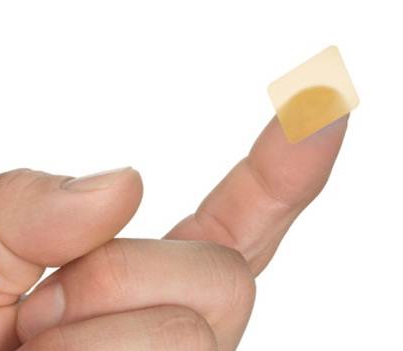
In 2015, a buccal formulation designed for absorption through the cheek became available. Belbuca film is quite convenient and comes in a moderate dose.
For intractable pain, a sublingual formulation of buprenorphine known as Subutex can be prescribed off label for pain. Subutex is also used to treat opioid addiction, but does not contain naloxone.
A Subutex tablet placed under the tongue takes about 20 minutes to be completely absorbed. Because buprenorphine binds to the pain receptors more tightly than any other opioid, the dose in milligrams required for full effect is much lower than similar strength morphine. Many medical researchers have concluded that buprenorphine is an excellent analgesic, with low risk for addiction or overdose. If taken as directed, the risk of respiratory depression from buprenorphine is the lowest of any opioid.
For pain relief, U.S. doctors must prescribe Subutex off-label, which means that they are prescribing for a condition that is not FDA approved. Subutex is approved for pain in Great Britain and most of Europe. The UK’s National Health Service recommends Subutex and other formulations of buprenorphine for patients “when weaker opioids for pain stop working.”
Of course, buprenorphine is not beneficial for every patient. And there is an issue of dental decay that requires careful monitoring and appropriate procedures. But for people in the most severe pain, who lack any other option because of the opioid prohibition mindset, buprenorphine may offer relief.
Finding a doctor willing to prescribe Subutex off label could be difficult. For severe or intractable pain that requires a high dose, a patient most likely needs to find a psychiatric or addiction treatment doctor licensed to prescribe buprenorphine in formulations such as Subutex that are pure buprenorphine.
Since 2000, the U.S. Congress has passed three laws that make buprenorphine more accessible to people with opioid use disorder. If Congress can aggressively lower the barriers to prescribing high-dose buprenorphine for addiction treatment, then why shouldn’t pain patients have access to medication that has the same dose of the active agent?
There is an education gap that prevents doctors and society at large from effectively managing this situation. The medical literature is heavily weighted toward studies of buprenorphine for addiction, with almost 97% of studies on opioid use disorder and less than 3% on pain. Pain patients also fear the stigma associated with buprenorphine as an addiction treatment, rather than an analgesic.
There is no objective reason for this. At the very least, buprenorphine should be an option for those forgotten patients who still live in pain. By overcoming the stigma of buprenorphine, doctors could treat patients with dignity by prescribing a safer and more effective medication.
Stefan Franzen, PhD, is a Professor of Chemistry at North Carolina State University. Franzen is the author of “Patient Z” – a book that looks at pain, addiction and the opioid crisis through the eyes of a patient who can’t find good pain care. He recently published a sequel to Z’s story, called “Z’s Odyssey.”