Veterans More Likely to Have Chronic Pain
/By Pat Anson, Editor
Nearly one out of ten U.S. military veterans suffers from chronic severe pain, according to an extensive new survey that found the prevalence of pain higher in veterans than nonveterans, particularly in veterans who served during recent armed conflicts.
The survey by the National Institutes of Health provides the first national estimate of severe pain in both veterans and nonveterans.
The prevalence of severe pain – defined as pain that occurs "most days" or "every day" and bothers the individual "a lot" – was 9.1% for veterans and 6.4% for nonveterans.
“Our analysis showed that veterans were about 40 percent more likely to experience severe pain than nonveterans,” said Richard Nahin, PhD, lead author of the analysis.
“Younger veterans were substantially more likely to report suffering from severe pain than nonveterans, even after controlling for underlying demographic characteristics. These findings suggest that more attention should be paid to helping veterans manage the impact of severe pain and related disability on daily activities.”
The study is based on data from a survey of over 67,000 adults (6,647 veterans and 61,049 nonveterans) who responded to questions about the persistence and intensity of their pain. The vast majority of veterans were men (92%), while most of the nonveterans were women (56%). The survey did not identify any specific aspects of military service, including branch of the armed forces, years of service, or whether the veteran served in a combat role.
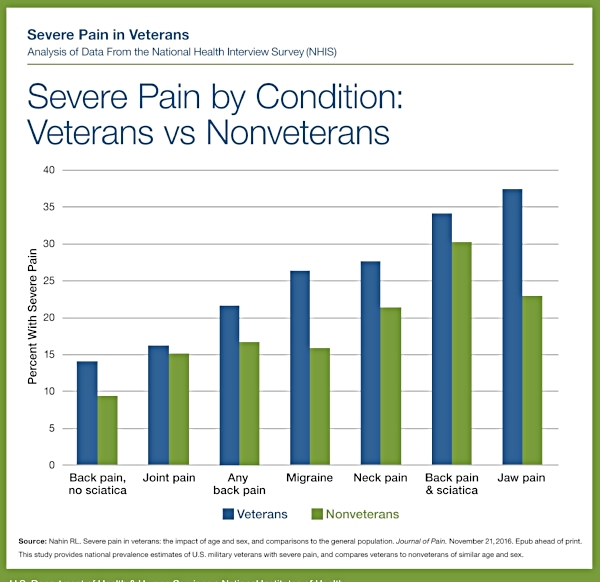
More veterans (65%) than nonveterans (56%) reported having some type of pain in the previous three months. They were also more likely to have severe pain from back pain, joint pain, migraine, neck pain, sciatica and jaw pain.
Younger veterans (8%) were substantially more likely to suffer from severe pain than nonveterans (3%) of similar ages.
“These findings show that we still have much more to do to help our veterans who are suffering from pain,” said Josephine Briggs, MD, director of the National Center for Complementary and Integrative Health (NCCIH). “This new knowledge can help inform effective health care strategies for veterans of all ages. More research is needed to generate additional evidence-based options for veterans managing pain.”
Veterans Complain About VA Pain Care
The survey adds to the growing body of evidence that military veterans are more likely to suffer from physical and mental health issues, and that their problems are not being adequately addressed by the Veterans Administration, which provides health services to 6 million veterans and their families. According to a recent VA study, an average of 22 veterans commit suicide each day.
One of them was Peter Kaisen. In August, the 76-year old Navy veteran committed suicide outside a VA Medical Center in Northport, New York. Kaisen’s widow told Newsday that her husband had chronic back pain, but VA doctors had told him there was nothing more they could do to ease his suffering.
According to a 2014 Inspector General’s study, more than half of the veterans being treated at the VA have chronic pain, as well as other conditions that contribute to it, such as depression and post-traumatic stress disorder.
In recent months, dozens of veterans have complained to Pain News Network that their treatment grew worse after the VA adopted the Centers for Disease Control and Prevention’s opioid prescribing guidelines, which discourage doctors from prescribing opioids for chronic pain.
“I am a Vietnam era veteran who has had testicular cancer, prostate cancer, hip joint cancer, and have been living with an inoperable spinal cord tumor,” wrote Tommy Garrett. “I cannot get the VA to prescribe OxyContin that civilian doctors have had me on for 17 years.”
“I received epidurals for 10 years and also I received pain medication for 6 years. The VA quit giving me epidurals and also took me off Vicodin,” said Mitch Kepner. “(Before) I was active and now I just lay around and do nothing wishing I was dead. I have no life, everything I do is a struggle. I don't want pity. I don't want compassion. I don't want (anything) from anybody. I just want Vicodin back so I can function.”
After several years of taking morphine to relieve pain from chronic arthritis, Vietnam veteran Ron Pence had his dosage cut in half by VA doctors – who want him to take Cymbalta, a non-opioid originally developed to treat anxiety. After reading about Cymbalta's side effects, Pence refused to take it.
“Why start something like that when what I was taking had no side effects for me and was working fine? I am sure the pills they are pushing will end in a lot more deaths and terrible disabilities and suffering,” wrote Pence in a PNN guest column.
“We are in one of the most advanced countries in the world medically, yet the doctors and politicians will not use that knowledge to ease pain and suffering. We have to find a solution.”