Chronic Pain Linked to Memory Loss in Some Older Adults
/By Pat Anson, PNN Editor
A new study suggests that people who live with chronic pain may be at higher risk of memory loss and cognitive decline if they have lower levels of education, income and access to healthcare.
The study by researchers at the University of Florida, published in the Journal of Alzheimer’s Disease, involved 147 adults between the ages of 45 and 85 who had mild to moderate knee pain. Participants enrolled in the study were asked to provide sociodemographic information, complete an assessment of their cognitive function, and have MRI brain scans.
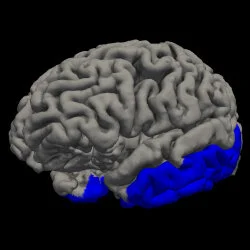
People with higher pain levels who had low levels of income and education, and less access to health insurance had about 4% less gray matter in the temporal lobe of their brains (the area shaded in blue) compared to people with low pain levels who had more income and education, and greater access to healthcare.
“As we get older, typically starting around our mid-50s to mid-60s, we lose about half a percent of our gray matter per year,” said lead author Jared Tanner, PhD, an assistant professor of clinical and health psychology in the UF College of Public Health and Health Professions. “So a 3-4% difference could be thought of as an additional six to eight years of aging in the brain.”
The thinning of gray matter is predictive of future cognitive decline and greater risk of developing dementia or Alzheimer’s disease.
Tanner and his colleagues have been investigating how chronic pain acts as a stressor that causes physiological changes in humans. Other researchers have found that Black adults are up to twice as likely as White adults to develop Alzheimer’s disease. The new findings indicate a variety of environmental factors might be involved, including access to healthcare.
“This study helps us begin to identify an additional factor to explore that may contribute to health disparities in rates of dementia and Alzheimer’s disease in some underrepresented ethnic/race groups. In this case, it looks like stage of chronic pain, along with other life experiences, may be playing a role,” said Tanner.
“The body and the brain are adaptive to stress to a certain point,” said senior author Kimberly Sibille, PhD, an associate professor of aging & geriatric research and pain medicine in the UF College of Medicine. “But with persistent stressors that are more intense and longer duration, eventually the body’s response is no longer adaptive and changes start occurring in the other direction, a process known as allostatic overload.
“People with low pain stage — intermittent, low intensity, shorter duration and minimal sites of pain — differ from the groups with higher stages of chronic pain. Further, in combination with lower protective factors, including lower income, education and health insurance access, those individuals with higher chronic pain stage show less gray matter in cortical areas of the brain.”
A large 2017 study found that people aged 60 and older with chronic pain had faster declines in memory and cognitive ability than those who were not troubled by pain.
The brain may be able to regain some of its ability to function normally. A 2009 study of osteoarthritis patients showed a reversal in brain changes when their pain was adequately treated.