Lupus May Be Caused by Common Virus
/By Graham Taylor and Heather Long
Around 5 million people worldwide live with the autoimmune condition lupus. This condition can cause a range of symptoms, including tiredness, fever, joint pain and a characteristic butterfly-shaped rash across the cheeks and nose.
For some people, these symptoms are mild and only flare-up occassionally. But for others, the disease is more severe – with constant symptoms
Although researchers know that lupus is caused by the immune system mistakenly attacking the body’s own tissues and organs, it isn’t entirely clear what triggers this response. But a new study suggests a common virus may play a key role in lupus.
There are two main forms of lupus. Discoid lupus primarily affects the skin, while systemic lupus erythematosus – the most common form of lupus – is more severe and affects the organs.
The immune system’s B cells play a key role in systemic lupus. B cells normally produce proteins called antibodies to target pathogens such as viruses and bacteria. But in people with systemic lupus, some B cells produce antibodies, called autoantibodies, that instead bind to and damage their own organs.
What causes B cells to produce autoantibodies in people with systemic lupus is poorly understood. But this recent study suggests that the trigger may be a common virus.
EBV Infection
Epstein-Barr virus (EBV) infects most people worldwide. Infection with EBV most commonly occurs in childhood, when it usually goes unnoticed. But if a person becomes infected by EBV in adolescence, it can cause infectious mononucleosis (better known as glandular fever).
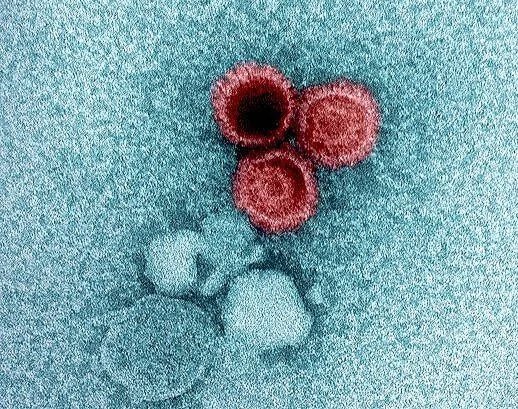
EBV is a type of herpes virus. These are complex viruses that are able to escape the body’s immune response by hiding inside certain cells.
In these cells, herpes viruses switch off their genes and go silent – like submarines diving beneath the waves to hide from the enemy. This allows herpes viruses to persist throughout a person’s lifetime – occasionally reawakening to spread to new people.
Interestingly, EBV has evolved to hide within the immune system itself, infecting and persisting in a very small number of B cells.
This strategy has proven highly successful for EBV. Over 90% of adults around the world are infected with EBV – meaning the virus is hiding in their immune system’s B cells.
EPSTEIN-BARR (ebv) VIRUS
While most people experience no adverse consequences from their infection, EBV has been linked to certain diseases.
For instance, EBV was the first virus shown to cause cancer. Subsequent research has linked EBV to several different types of cancer – including certain lymphomas and 10% of stomach cancers. Each year, about 200,000 people develop an EBV-associated cancer.
More recently, large epidemiological studies have linked EBV with multiple sclerosis, which is an autoimmune condition. Studies have shown that people with multiple sclerosis are almost always infected with EBV.
Previous research has also suggested that EBV may be involved in systemic lupus. But this new study provides insight into the specific mechanism involved.
To conduct their study, the researchers developed a sensitive test to analyse the genetic material in thousands of B cells isolated from the blood of people with systemic lupus and healthy donors as a control.
They found that EBV was present in around 25 times more B cells in systemic lupus patients compared to participants who didn’t have the condition. In systemic lupus patients, EBV was present in around one in 400 B cells – while in healthy controls it was only present in around one in 10,000 B cells.
This is an interesting finding – though the researchers acknowledge it could potentially be caused by the medicines patients with systemic lupus take to control their illness. These decrease the activity of the immune system which reduces the symptoms of systemic lupus. But these medicines also reduce the immune system’s ability to control EBV infection.
How EBV Causes Autoimmunity
The most important finding from the research was that many of the EBV-infected B cells from systemic lupus patients made autoantibodies that bound to specific proteins. These same proteins are often targeted by autoantibodies in people with systemic lupus. In contrast, EBV-infected B cells from healthy donors did not make these autoantibodies.
To understand the mechanisms involved, the researchers then studied the expression of EBV genes in the infected B cells. Although EBV was generally shown to be in its silent state, some EBV-infected B cells from systemic lupus patients produced the viral protein EBNA2, which reprogrammed the B cells to become more inflammatory. These activated B cells were better able to stimulate responses from other immune cells, including non-EBV infected B cells and T cells.
Together, these observations suggest that EBV may initiate systemic lupus by infecting and reprogramming dormant B cells to become activated. These cells produce autoantibodies that could potentially contribute to the development of systemic lupus. They also appear to recruit additional immune cells able to produce stronger autoimmune responses that are more likely to play a role in systemic lupus development.
These new findings raise the possibility that targeting EBV could form the basis of a new therapy to treat people with systemic lupus. But given these infected B cells also recruit additional immune cells, a broader therapeutic strategy may be needed.
Additional research will also be needed to confirm whether EBV is indeed an essential trigger for the development of systemic lupus. If this is confirmed, preventing EBV infections through vaccination could prevent systemic lupus developing.
Currently there are a number of potential EBV vaccines in development – and two candidates are being tested in large clinical trials. A key requirement for any effective EBV vaccine will be its ability to generate long-term protection against infection. This is because EBV is already widespread in the population. If vaccination only delays infection until later in life, then this could lead to many cases of glandular fever.
The results of these trials are eagerly anticipated, given the potential impact an effective vaccine could have to reduce the numbers of people worldwide that develop lupus, other autoimmune conditions, or cancers caused by EBV.
Graham Taylor, PhD, is an Associate Professor in Viral and Tumour Immunology at the University of Birmingham. The main focus of Graham’s work is to increase our knowledge of the immune system in health and disease and how best to harness the immune system to treat cancer. His research helped lead to a therapeutic cancer vaccine that has undergone testing in several clinical trials.
Heather Long, PhD, is an Associate Professor in the Department of Immunology and Immunotherapy, at the University of Birmingham. She leads a research team in the fields of viral and cancer immunology, with a long-term focus on understanding T cell control of viruses and virus-associated cancers.
This article originally appeared in The Conversation and is republished with permission.