Message to CDC: Tear Down Your Walls of Silence!
/By Richard Lawhern, PhD, Guest Columnist
In March 2016, the Centers for Disease Control and Prevention published its guideline for primary care physicians on prescribing opioid medication for chronic non-cancer pain.
Three months before its publication, Congress and President Obama made the guideline mandatory for the Veterans Health Administration, leading to revised practice standards at the VA that sharply restrict opioid medication for all veterans, regardless of risk or benefit. These unjustified restrictions were again written into federal law by the Veterans Administration Mission Act and recently signed into law by President Trump.
In civilian practice -- and despite being phrased as voluntary and only for general practitioners -- the CDC guideline was immediately and widely interpreted as a mandatory standard of practice for all doctors.
Many insurers and healthcare providers adopted the CDC’s 90mg morphine equivalent dose (MME) as the maximum safe level of treatment, and some states have limited opioids to 7 days' supply or less for initial prescriptions, even after major surgery.
More recently, Oregon’s Medicaid program has proposed rule changes that would forcibly taper many chronic pain patients currently on opioid therapy to zero.
Major changes are also coming next year for Medicare patients nationwide that will sharply restrict high-dose opioid therapy for hundreds of thousands of older and disabled patients, by allowing insurers to require prior authorization for prescriptions in excess of 200 MMEs.
Almost immediately -- and despite wording in the CDC guideline discouraging such action -- doctors began coercing patients to eliminate or reduce opioids that were effective in managing their pain for years. State and federal law enforcement agencies like the Drug Enforcement Administration also ramped up the investigation and prosecution of doctors who prescribe high doses.
Fearing loss of their livelihoods, many doctors refused to prescribe opioids or discharged patients who asked for them. Some physicians left pain practice altogether. As a result, tens of thousands of patients can no longer find effective pain treatment. There are widespread stories in social media, acknowledged in professional medical literature, of patients deserted by doctors who spiral down into agony, disability, and in some cases suicide.
Where is CDC’s Guideline Evaluation?
One would think that federal agencies that caused such a public health disaster would be concerned with correcting course. But that is not the case.
Practice standards published by medical associations usually include a follow-up program to measure their safety and effectiveness. However, CDC has failed to conduct a full assessment of the opioid guideline in the nearly two and a half years since its release – even though the agency pledged in the guideline to conduct one:
“CDC is committed to evaluating the guideline to identify the impact of the recommendations on clinician and patient outcomes, both intended and unintended, and revising the recommendations in future updates when warranted.”
It is obvious why the CDC has maintained a wall of silence in the face of widespread criticism of the guideline by both patients and doctors. The agency is desperately wrong on three central assumptions about the opioid crisis:
- The crisis was caused by “over-prescribing” medical opioids to patients in pain. Doctors were careless, greedy or deceived by evil pharmaceutical companies into ignoring risks of drug addiction.
- There is no evidence that opioid analgesics are effective for pain when used over long periods.
- Alternative pain therapies and non-opioid medications are safer and more effective than opioids and should be preferred over them.
All three of these assumptions are wrong. Patient experience and published data from healthcare researchers demonstrate they are wrong. Let’s look at these three false assumptions.
Do Opioid Prescriptions Cause Overdose Deaths?
Very rarely. If prescribing increases the risk of opioid overdose deaths, then we would expect to see more overdoses in states and patient demographic groups where prescribing rates are highest. But we do not.
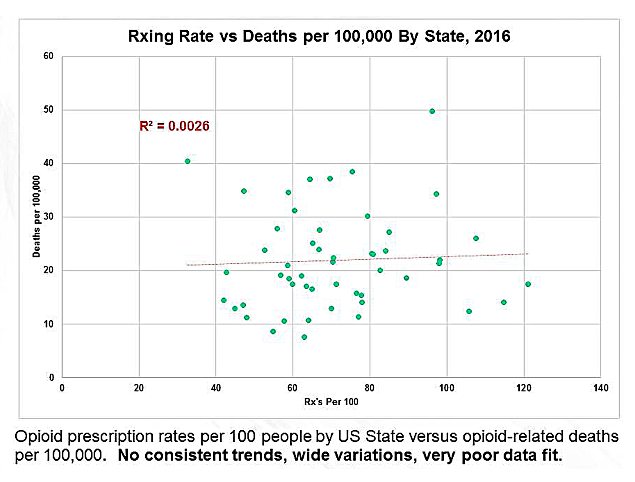
The following graphic compares overdose mortality rates from legal and illegal opioids to rates of opioid prescribing in all 50 states and Washington, DC in 2016.
SOURCE: CDC DATABASE
It might be difficult for a layman to make much sense of this graphic. And that is precisely the point. If there was a clear cause and effect relationship between prescribing and overdose deaths, then we would see higher death rates on the right side of the chart, with most data clumped closely around a rising central trend line. But we don’t see that.
The contribution of medically prescribed opioids to overdose deaths is so small that it gets lost in the noise of illegal street drugs. Contrary to the screaming headlines in the media, prescription drugs aren’t killing people in large numbers. Illegal street drugs are.
This is not to say prescription drugs played no role in worsening the opioid crisis. But in recent years, their role in opioid mortality has become small. Even when they are found in the bloodstream of an overdose victim, opioid prescriptions are almost never found alone. In Massachusetts, illicit fentanyl was found last year in 85% of blood toxicology screens of overdose victims, while heroin and/or cocaine were detected in about 45% of them. Prescription opioids were found in only 15% of overdose victims.
Those numbers obviously don’t add up to 100 percent. That is because the great majority of overdose victims had taken more than one illegal drug plus alcohol and/or benzodiazepine drugs. We don’t really know which drug or combination of drugs caused the overdose.
Overdose data also suggest that death is not a predictable outcome of opioid prescribing, nor is it common in groups that use the most opioid prescriptions.
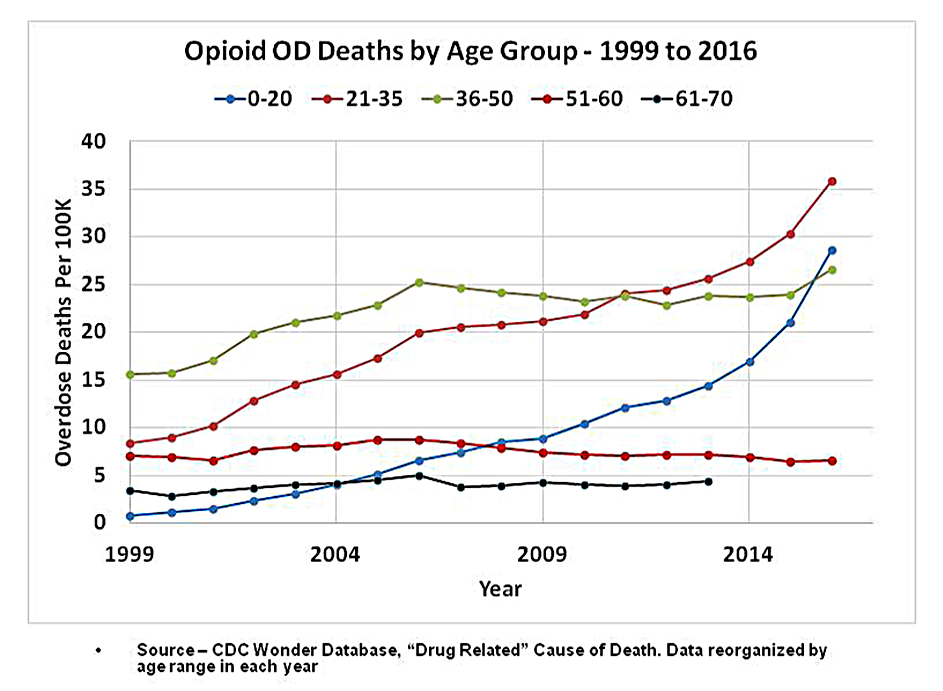
Basic trends in the chart below stand out. First, rates of overdose deaths among people over age 50 have been stable for the last 17 years, while death rates among young people have risen sharply. In 2016, they were six times higher than in seniors.
We know that rates of opioid prescribing for seniors are at least 250% higher than for kids under 21. Thus, the group that benefited the most from liberalized prescribing policies of a decade ago – older adults -- has shown no higher risk of overdose deaths, even as kids who receive fewer opioid prescriptions are now dying in record numbers.
The asserted demographics of “over-prescribing” are plainly wrong. They don’t work and never have. Exposure to medically managed opioids does not cause increased opioid mortality, at least not directly.
Brief exposure to prescription opioids contributes very little to addiction or long term use. In two recent large-scale studies, opioid abuse and prolonged prescribing of opioids were evaluated for over 650,000 patients given opioids for the first time to control pain after surgery. Fewer than 0.6% of these patients were diagnosed with opioid abuse 2.5 years later.
This means that opioid treatment for acute pain is safe, effective and usually free of bad outcomes for over 99% of opioid-naive post-surgical patients.
Do Opioid Medications Relieve Chronic Pain?
Of course they do!
We hear a lot of noise that there is no evidence or proof that opioids work for long periods. But “no proof” is not the same as “proof of no effect”.
There are very few double blind clinical trials for opioids longer than 90 days -- and this reality is entirely understandable. When people with severe pain are given placebos, they lapse into agony and drop out of trials. Long term studies of any pain treatment can easily rise to the level of being inhumane – which is why so few have been conducted.
It isn’t rocket science, and the writers of the CDC guideline knew it. Instead of comparing shorter trials of opioid analgesics against behavioral therapies and non-opioid medications, the guideline writers stacked the deck against opioids. And they got caught at it by their medical peers.
If trials of all three therapies had been limited to studies of at least a year -- as opioids were but alternative therapies were not -- none of the three could have provided “evidence” of useful effect.
We must also acknowledge that not all patients do well on opioids. Some develop persistent nausea, sedation, constipation, suppression of sexual libido and depression. Some patients also become drug tolerant, requiring ever-increasing doses of opioids to achieve the same pain-relieving effects. It has been theorized that a condition called “opioid induced hyperalgesia” may alter the action of opioid receptors in the brain. But there is no medical consensus on how to measure such an effect in human beings, or even whether hyperalgesia exists.
Many of the perceived failures of opioid therapy might be laid at the feet of ill-trained physicians. Some doctors titrate their patients from zero to a therapeutic dose too fast. Others fail to recognize factors in liver metabolism which make some patients poor metabolizers or hyper-metabolizers of opioids. Variation in metabolism means that there can be no one-size-fits-all pain treatment. Opioid therapy can be safe and effective for a small minority of patients at doses well above 1,000 MME.
Are Safe Substitutes for Opioids Widely Available?
For millions of patients, not yet.
We hear a lot of noise about tapering pain patients out of opioid therapy and into “alternative” or “integrative medicine.” Indeed, it seems appropriate to first try less powerful medications such as NSAIDs or anticonvulsants before proceeding to opioids. Exercise and massage therapy are also useful as palliative therapies. But for millions of people, less powerful medications don’t work well enough -- or at all. Tylenol or ibuprofen at high doses might also put you in a hospital with liver toxicity or major gastrointestinal problems.
What about “non-pharmacological” and “non-invasive” therapies? Do they work well enough to be substituted for opioids? Unfortunately, the answer is no. The state of science for alternatives like cognitive behavioral therapy, acupuncture, chiropractic, or various talk therapies is simply abysmal.
At most, these alternative treatments are experimental. They might be useful as supportive therapies in coordination with a well managed program of pain relieving medications. But pending a more rigorous evaluation, we simply cannot offer such experimental techniques as substitutes for opioids.
What Are Federal Agencies Doing to Correct Course?
In two words, “nothing apparent.”
The CDC, Food and Drug Administration, Health and Human Services (HHS), and the National Institutes of Health seem to be collectively dragging their feet in a campaign of deliberate inaction, refusing to respond to criticism or examine their own medical evidence of error.
This author and others have been trying for years to get healthcare agencies to reevaluate the relationship between opioid prescribing and overdose mortality. These efforts have included recent testimony to the FDA Opioid Policy Steering Committee and to the HHS Inter Agency Task Force on Best Practice in Pain Management.
In addition, copies of our analysis have been sent to the following authorities. Most have been silent and none have responded in substance.
- Dr. Scott Gottlieb, FDA Commissioner and senior analytics staff
- Dr. Sharon Hertz, Director, Division of Anesthesia, Analgesia, and Addiction Products, FDA
- Dr. Mary Kremzner, Director, Division of Drug Information, FDA. (Dr. Kremzner responded with a courteous letter referring to a press release from Scott Gottlieb).
- Alicia Richmond Scott, Designated Federal Officer, and Dr. Vanilla Singh, Chair of the HHS Inter Agency Task Force on Best Practices in Pain Management
- Dr. Nora Volkow, Director of the National Institute on Drug Abuse
- The Whistleblower gateway of the House Subcommittee on Government Oversight
An inquiry was also filed online with the CDC. A dismissive response was received from the CDC Center for Injury Prevention – which oversaw development of the opioid guideline -- claiming to have read my analysis and asserting their previous positions. This response was clearly a brush-off adapted from previous form letters.
A request is now in preparation to the HHS Office of the Inspector General, asking for investigation of CDC for malfeasance and possible fraud.
Richard Lawhern, PhD, has for 21 years volunteered as a patient advocate in online pain communities and a subject matter expert on public policy for medical opioids. He is co-founder and corresponding secretary of the Alliance for the Treatment of Intractable Pain.
Graphics in this article originally published by The Crime Report on January 21, 2018, in "The Phony War Against Opioids - Some Inconvenient Truths."
The information in this column should not be considered as professional medical advice, diagnosis or treatment. It is for informational purposes only and represents the author’s opinions alone. It does not inherently express or reflect the views, opinions and/or positions of Pain News Network.