New Website Launched for Kratom Comments
/By Pat Anson, Editor
In a sign of their distrust of the federal government, kratom community activists have created their own website for supporters to submit comments to the U.S. Drug Enforcement Administration on the proposed classification of kratom as a controlled substance.
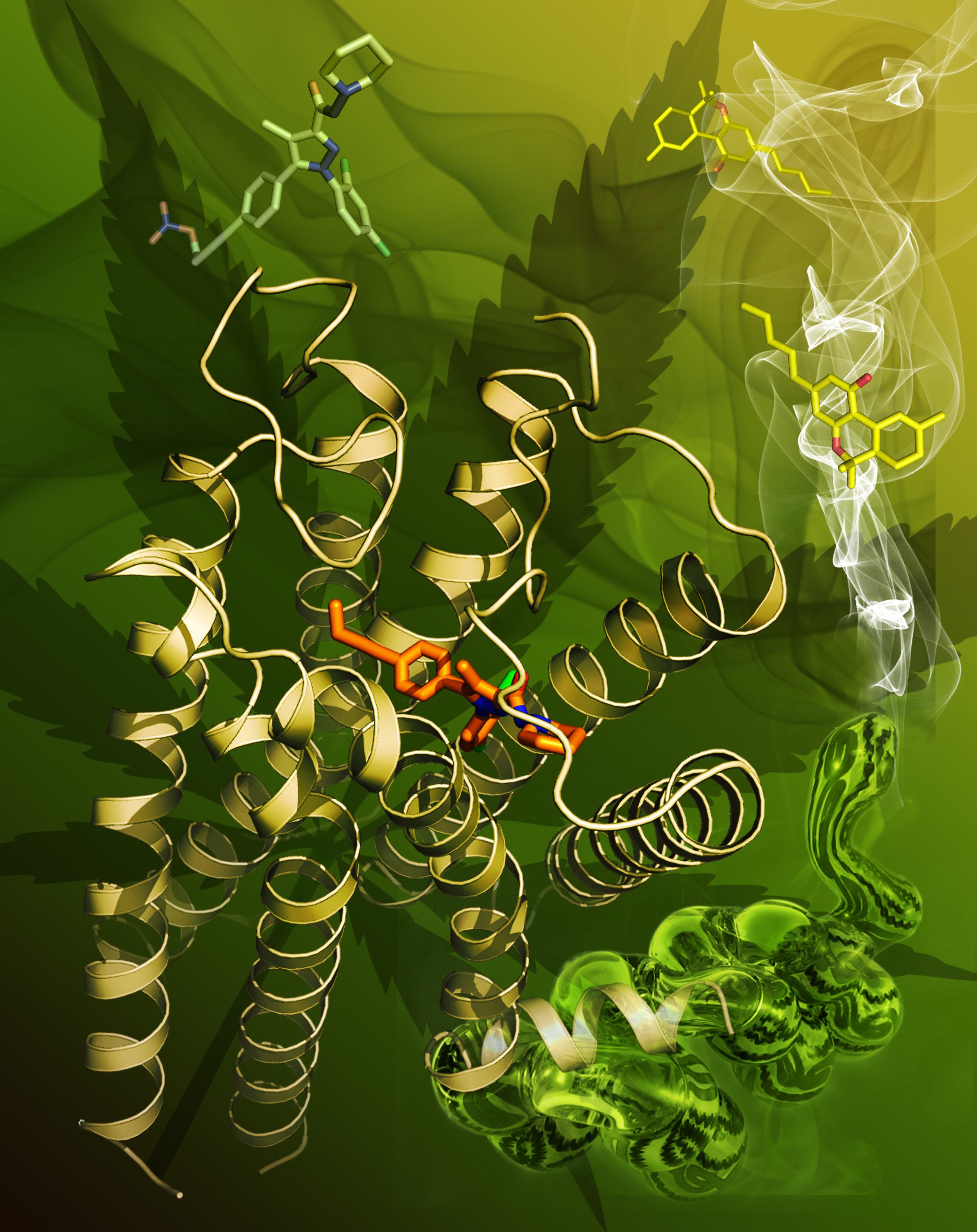
On October 12, the DEA formally withdrew its controversial plan to classify two of the active ingredients in kratom as a Schedule I substances, which would have made the sale and possession of the herb a felony. Instead, the DEA said it would ask the Food and Drug Administration for a full medical and scientific evaluation of kratom, and solicit public comments on the issue at Regulations.gov.
But issues arose almost immediately with the Regulations.gov website, where some kratom supporters said their comments weren’t accepted or the website was having technical difficulties.
Similar problems were reported when the Centers for Disease Control and Prevention took comments at Regulations.gov on its opioid prescribing guidelines. In the end, over 4,000 comments on the guidelines were received, a record number.
This week the American Kratom Association (AKA) and the Botanical Education Alliance launched KratomComments.org to take comments from the public that will then be automatically submitted to Regulations.gov with an independent record of their submission. Software used by the website was created by The Soft Edge, Inc. (TSE) to avoid some of the pitfalls of Regulations.gov.
“KratomComments.org is the best way of protecting the kratom community,” the AKA said in a statement. “No comments can be ‘lost’ due to glitches at Regulations.gov. That site has been down already and no one knows what was lost. KratomComments.org ensures that comments made will be independently stored and recorded.
“There is no track record whatsoever of submissions made through TSE platforms to Regulations.gov being rejected. To the contrary, the platform has been used to facilitate the successful submission of several hundred thousand comments.”
But not everyone is on board with a third party submitting comments to the government.
“If you use the American Kratom Association’s ‘kratomcomments.org’ you are risking your comment not being counted,” warns kratom supporter Levi Beers on his website. Beers said he was advised by the DEA to submit comments directly to Regulations.gov and not through a third party.
“People are so confused you’ve got people submitting comments through regulations.gov and kratomcomments.org, which is going to hurt this process,” Beers said.
Hundreds of Comments Submitted
So far, over 800 comments have been submitted to Regulations.gov. The vast majority are from people who say kratom – which comes from the leaves of a tree in Southeast Asia – has helped them manage symptoms of chronic pain, anxiety, depression or addiction.
“Kratom has allowed me to live a highly productive, healthy and enjoyable life after my personal journey through addiction,” wrote Troy Foos, a 51-year old man who said he was addicted to alcohol and opioid pain medication.
“My life, my marriage and my relationship with my kids is a thousand times better because of the 'helping hand' of this plant. Similar to how two cups of coffee get me rolling in the morning, it has allowed me to successfully navigate my addictions and live a healthy, highly effective life at work and at home.”
“As a person with chronic pain caused by fibromyalgia, having kratom as a non-addictive option has been great,” wrote Wyatt Gaylor. “I can now take it when I'm having a bad day without the side effects associated with opiates.”
“Kratom definitely needs to be banned,” wrote an anonymous poster who left one of the few negative comments about kratom. “My son is currently in rehab for addiction to kratom. This is a very serious product which has caused very serious health issues in someone who is only 20 years old.”
There is usually a discrepancy at Regulations.gov between the number of the comments received and the number posted. That’s because comments are not posted until the next business day. Others are under review by DEA because of personal information or inappropriate language. Comments will be accepted until December 1, 2016.