Still, the media often portrays pain patients as drug seekers.
Meanwhile, people are overdosing on fentanyl because it’s being mixed with other common street drugs. Three grains of fentanyl are considered a lethal dose, indicating its potency, and Mexican drug cartels have figured out that it’s much cheaper for their enterprise. It was a business decision that has led to many deaths.
Let’s pretend that the vast majority of chronic pain and illness patients are diligent and responsible. Let’s pretend all of these issues are separate. Let’s pretend that drug addiction and drug dependence are two different things.
I’m going to run you through my day as an opioid-dependent human being.
For your reference: I have chronic back and neck pain stemming from two separate car accidents. I broke my thoracic spine in four places, one of which healed incorrectly and calcified over a cluster of nerves. This means that every movement of my midsection feels like someone is hammering nails directly into my spine. The second car accident necessitated two cervical fusions. If I stretch my neck any more than necessary, I get headaches so intense that they send me back to bed.
Using a straight 1 to 10 scale, 1 being the best level of pain, 10 being the worst, I live my life at a constant 7/10. On good days I can get down to 5/10. So, imagine having someone standing behind you all day, every day, screaming into your ear and tasing you endlessly. That’s my typical day.
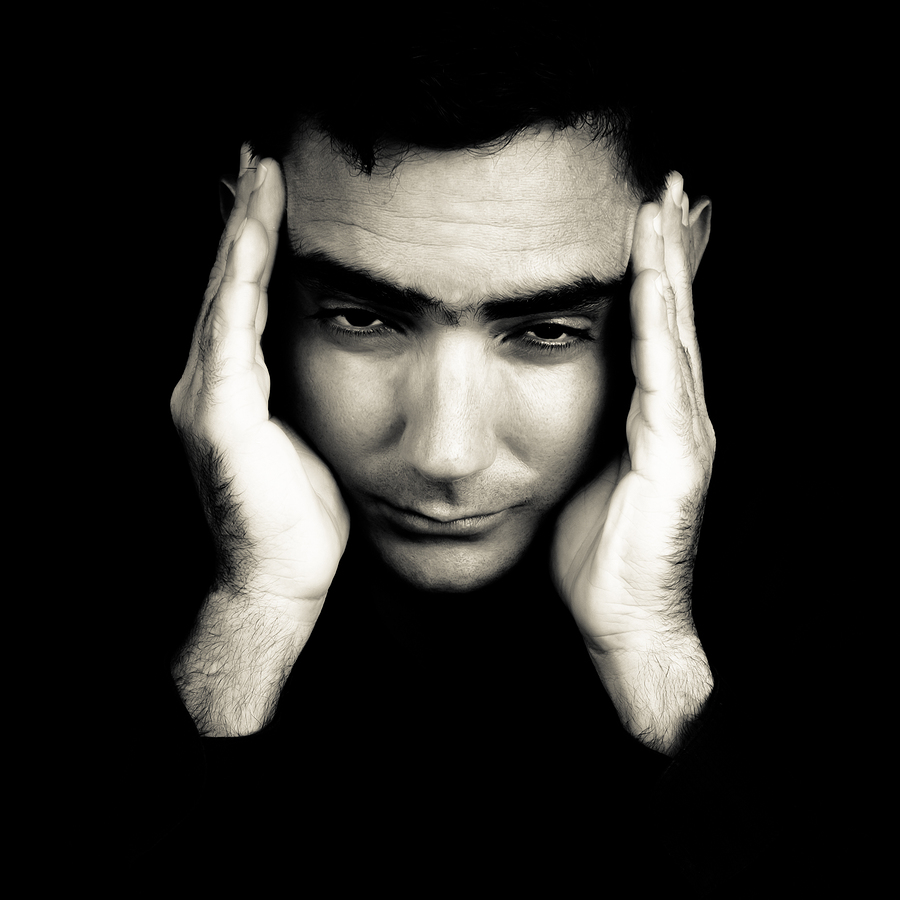
This is an example of what an opioid-dependent person looks like:
7 am: I wake up. I’ll get dressed, put on my beloved Quell pain relief device (which, for the record, I bought myself during their Indiegogo campaign last year), and head downstairs for coffee. First I will drink UltraInflamX 360, an anti-inflammatory medical powder. It is expensive and lasts for 14 meals. If I don’t eat it, my esophagus is raw and painful because of eosinophilic esophagitis, an autoimmune condition that causes food-allergy-like responses, and GERD. Nobody is sure why I have these, except that all of the medications I take have the potential to destroy my gastrointestinal tract.
Then I take the following medications:
- Tramadol (synthetic opioid)
- Lyrica (nerve medication)
- Duloxetine (antidepressant used off-label for pain control)
- Prilosec (protects my GI tract and helps with GERD)
- Multivitamin (always a good idea)
- Calcium
- Vitamin K2
- Vitamin D3 (used to offset the bone-weakening properties of Prilosec)
- Turmeric (anti-inflammatory properties)
7:30 - 8 am: I drink coffee and catch up on emails. Typically, I sit in my recliner chair with a body-length heating pad. Today I also have an ice pack on my neck because I didn’t sleep last night. Being in complete spasm will do that to you.
8 am - 12 pm: I work. I had to leave my law firm at the end of 2015 because I could not physically handle an office job. Now I work from my recliner and telecommute part-time for a few different companies. I am trying to transition into our home office and use a kneeling chair. During these three hours I get up multiple times, stretch, do gentle yoga, and think about lunch.
Noon - 1 pm: Lunch. I used to take another Tramadol at the four-hour mark, but lately I have been trying to hold off most of the day. It is important to note here that opioid-dependent patients occasionally test how long we can go without meds (if we feel up to it). We don’t like being dependent. That is why I constantly test my boundaries. These days I can make it to 6 pm without a second pill. On bad days, I need to take one pill every four to six hours -- which is actually what my doctor instructed.
1 pm - 2 pm: I take a walk outside while listening to podcasts or audiobooks. Since I can’t hold books comfortably (my neck doesn’t like it when I look down), I listen instead.
2 pm - 4 pm: I try to do some more work. This can be hit or miss depending on how much pain I have on any given day. If I am in too much pain, I stretch or watch television from the recliner.
4 pm - 6 pm: Power-down time. I sit in the recliner and read interesting articles, look at the news, and find cute animals online. Some days I’ll wear a soft cervical collar to take stress off my neck.
6 pm - 8:30 pm: My husband comes home and we spend time together.
8:30 pm - 9 pm: My husband reads while I begin the very long process of getting ready to sleep. This includes taping Lidocaine patches on my back. I can only put on three at a time and I have a lot of real estate to cover, so I place them on the loudest areas for that specific day. Then I take the following medications:
- Tramadol
- Duloxetine
- Lyrica
- Methocarbamol (muscle relaxer)
- Zyrtec (allergies)
I also put Mederma on my cervical fusion scar in the hopes of making it fade. Then I sleep with two pillows under my knees so that my low back doesn’t keep me awake. When I sleep on my side, I keep a pillow between my legs. I have a cervical pillow for my neck.
That’s it. That’s the extent of opioid dependence. I need opioids to get through the day, but my day is not focused around them. On bad days I occasionally take two Tramadol at once, which my doctor recommended if I’m having a lot of pain. The numbers of times I do that per month can be counted on one hand because I don’t want to abuse it and lose access.
Would I take something stronger if my doctor prescribed it? Absolutely. Having this pain and trying to live a normal life is like having someone screaming right in your ear all the time. It’s always there in the background, dictating every decision I make.
This is responsible opioid use and what the majority of chronic pain patients go through, though many are prescribed stronger painkillers than I am and need to take them more frequently. Many have asked me how I survive with just Tramadol. The answer? I have to, because what happens if it’s taken away? Then I have nothing.
I’ve learned to live with this constant pain because of the current political climate. My doctor won’t prescribe anything stronger because he said that eventually it’ll lose its efficacy. I can understand that. But nothing is being done to help chronic pain patients besides demonizing us in the media and taking away our only options.
You can’t remove that sole option without having something to replace it. And no, I’m not talking about “deep breathing” and “positive visualization,” both of which have been recommended. I do both. I don’t do them in place of Tramadol. They complement Tramadol.
Congress is now contemplating an opioid tax to fund addiction recovery programs -- a noble goal, but this makes it even more difficult for chronic pain patients. Do you know how much of my household’s monthly budget is spent on medication? Too much. Far too much.
This is not healthcare. This is extortion.
Our healthcare system is already ruined. Doctors refuse to prescribe medication that patients legitimately need for fear of losing their licenses. Insurance companies try to get out of paying by making already expensive conditions even more expensive to treat. I am a very expensive person to keep alive and functioning. Many, many people have it worse than I do.
The government and the medical system cannot take away our right to live. That is what opioid medication is for us: our right to live without pain. We must be separated from the current hysteria. There are millions of us in the United States alone.
We are not the monsters here. We are human beings who suffer indescribable agony on a daily basis, and we deserve to be protected.